¡Estamos aceptando nuevos clientes!
Todos los servicios se brindan independientemente del seguro o la capacidad de pago.
**Nadie será enviado a cobranzas por no pagar facturas**
Lyon-Martin Accepted Coverages
Medi-Cal and Medi-Cal Managed Care Plans:
‘Straight’ Medi-Cal (full scope Medi-Cal with no managed care plan; not emergency Medi-Cal)
Medi-Cal Anthem Blue Cross with: Lyon-Martin Community Health Services
- If you do not have listed as your provider with Anthem, you can call Anthem at (800) 407-4627 to request a provider change. Our clinic code is CV6000.
San Francisco Health Plan with: Lyon-Martin Community Health Services
- If you do not have listed as your provider with San Francisco Health Plan (SFHP), you can call SFHP at (415) 547-7818 to request a provider change. Our clinic code is 26507.
Health Plan of San Mateo (HPSM) with: Lyon-Martin Community Health Services or Special Member Status
- To request us as your primary care provider, complete this form and send it to us: https://www.hpsm.org/docs/default-source/provider-forms/epo_provider_selection_form.pdf?sfvrsn=80521dfb_15
- To request special member status, see below §
- If you do not have special member status, you can go to your assigned primary care provider (PCP) with HPSM to request a referral to us for gender affirming care.
Alameda Alliance with: Lyon-Martin Community Health Services
- If you do not have listed as your provider with Alameda Alliance, you can call Alameda Alliance at (510) 747-4500 to request a provider change. Just let them know you go to Lyon-Martin Community Health Services for your medical care.
Contra Costa Health Plan (CCHP) with: Lyon-Martin Community Health Services or prior authorization
- We are still finalizing contracting/credentialing with Contra Costa Health Plan, however, once complete, you should be able to call 925-313-6000 to request our clinic as your primary care provider.
- For now, you can call a request continuity of care approval to continue seeing us if you saw us for a primary care visit in 2023. CCHP may call/contact the clinic to follow up after your request and will inform you if the request is approved within 30 days of your request.
- Please be aware that we are not highly familiar with the referral options in Contra Costa County and not well resourced/connected to the local community supports that may be available to you there. We recommend that patients receive their primary care in Contra Costa from a provider there in network and ask for a referral to come see us for your specialty care needs specifically (gender affirming care and/or sexual and reproductive health care).
Partnership Health Plan of California (PHP) with: Lyon-Martin Community Health Services or Special Member Status
- We are still finalizing contracting/credentialing with Partnership Health Plan, however, once complete, you should be able to call them to request us as your primary care provider. The plan will contact the clinic after your request to confirm that you have been receiving care from our clinic.
- For now, you can request special member status from Partnership Health Plan, and we can see you if you have special member status.
- To request special member status, see below §
- If you do not have special member status, you can go to your assigned primary care provider (PCP) with PHP to request a referral to us for gender affirming care.
- Please be aware that we are not highly familiar with the referral options in the counties that Partnership Health Plan represents and not well resourced/connected to the local community supports that may be available to you there. We recommend that patients receive their primary care in their local county from a provider there in network and ask for a referral to come see us for your specialty care needs specifically (gender affirming care and/or sexual and reproductive health care).
If you do not have the option to switch to one of the managed care plans above, please check with your current managed care plan about local options for gender affirming care! If they cannot help you find an option, you can ask about special member status so you can come to our clinic for care or ask your insurance-assigned primary care provider for a referral to specialty care with our clinic.
§ Special member status allows someone to be a member of their current plan, but without a designated primary care provider, allowing them to go to many providers more easily.
We have seen patient successful gain special member status from a managed care plan for one of two reasons:
- Continuity of Care – Informing the plan that the patient already has established primary care with our clinic. This is designed to give patients already connected to care elsewhere 12 months to arrange transfer of their care to another provider in network.
- Gender Affirming Care – If the health plan does not cover a clinic that can provide competent healthcare of this kind, they must cover gender affirming care out of county.
You must call yourself to request this change in status, but we can help you make this call if you want assistance. Here are some tips:
- Call the customer service number on the back of the insurance card or go to DHCS website above for the plan number.
- Tell the health plan that you have been receiving services at Lyon-Martin and are requesting special member status for continuity of care.
- The representative may not know the process for obtaining special member status. That’s okay!
- Ask to speak with a supervisor who does know the process.
- They may tell you that you need to fill out “continuity of care” paperwork to obtain special member status. They should mail or email you the form and you can mail or fax it back to them.
- They may tell you that you need a referral from a clinic in to come to Lyon-Martin and obtain special member status. If this is the case, you must book a new patient appointment with your assigned primary care provider through your plan and request a referral from them.
- If you are seeking special member status for gender affirming care, and you have not been able to access that care through your plan, you can tell the representative: “Under California law, I need access to transgender care, and my insurance must cover that care. No one in-network offers transgender care, but Lyon-Martin Health Services does. To provide adequate care and fulfill ‘network adequacy’, you must allow me to seek care where that can happen, and Lyon-Martin offers that care.”
- The representative may be able to help you find a clinic that can provide gender affirming care in your local area and that is already in-network with the plan. That’s great! You can also connect your local provider to TransLine, https://project-health.org/transline/, where they can connect to gender affirming care experts across the country.
Medicare Plans:
Medicare with: parts A and/or B AND NO Part C plan
- If your Medicare has a Part C plan, please see below about commercial plan acceptance.
Private or Commercial Coverage:
We accept all PPO-type insurance, however, please assume we are out of network, unless specified as in-network below. You can call your plan to check if we are an in-network provider.
If you have an EPO or POS or HMO plan, you do not have out-of-network benefits. Please confirm with your insurance that we are in-network before scheduling with us. If you have an HMO or EPO plan, you will need to confirm you can assign our clinic as your primary medical home or primary care provider. If not, you will need to see if you can get a referral from your assigned primary care provider to our clinic.
Aetna:
Elect Choice EPO
- In-network if with APCN_NCA_OASEL (Aetna Preferred Network Northern California Open Access Select), EPO Northern California, or NorCal EC Excl all Sutter (Elect Choice all Sutter)
Managed Choice
- In-network if with Nor CA MC Excl all Sutter (Northern California Managed Choice all Sutter)
Managed Choice POS
- In-network if with PCN_NCA_POSII (Preferred Choice Network Northern California POS II) or POS Northern CA
Open Choice PPO
- In-network if with No CA PPO Excl Sutter (Northern California PPO Sutter) or PPO Northern CA
Anthem :
- BC PPO Incentive (prefix FZE, LLZ, NKB) – In network
- Blue Access PPO (prefix BLBAN ) – In network
- CA (California) Blue HPN (High Performance Network) EPO – Out of network
- CA (California) Generic Health Savings (Prefix GGS) – In network
- CA (California) SG Anthem PPO (Prefix JQU) – In network
- CA (California) Medicare WLP (Well Plan) (prefix MMA, JQW) – Out of network
- California Care HMO (prefix JQK) – In network
- CT (Connecticut) Blue Card PPO (prefix DTU) – In network
- General Health Saving Account w/ Alt – In network
- Medi-Cal (prefix XDJ) – see below under Anthem Medi-Cal Blue Cross
- MO (Missouri) HSA PPO (prefix RWJAN) – In network
- Pathway EPO (prefix YZC, JBE)– Out of network
- PG&E PPO Health Account (prefix PZG) – In network
- PPO Incentive (prefix XDGCA, XDP) – In network
- PPO PB Classic (prefix YSQ, XDB) – In network
- PPO PB Incentive (prefix AQT, PDP, XDP, Z9M) – In network
- Prudent Buyer PPO (prefix JQU) – In network
- Select HMO (prefix JQV) – In network
- Select PPO (prefix JQY) – Out of network
- UC Care PPO (prefix VUC) – In network
There are numerous Anthem plans, and then names they use to describe themselves to us may differ from the name on your card. We highly recommend that you check directly with your coverage to confirm we are in-network for your specific plan.
Blue Shield:
Blue Shield of California PPO
- NOT in network Tandem or High-Performance Network
Hill Physicians:
- We are NOT in network with Hill Physicians.
Tricare:
- We are NOT in-network with any Tricare plans.
United:
- United PPO, EPO – NOT in network with any plans. Patients with EPOs can seek ‘gap coverage’ for our visits to be covered, but they will need to get an in-network provider to refer them to us and prior authorization from their plan for visits with us.
Other Coverage Programs:
Healthy San Francisco with: Lyon-Martin Community Health Services*
*Healthy San Francisco does not cover the cost of visits at the clinic, so clients should separately apply for our sliding scale discount program for a potential reduction on the cost of care provided at the clinic. Lab work is covered only if done at San Francisco General Hospital, so clients should go there for all laboratory testing.
- We can assist you in applying for or renewing this coverage!
Every Woman Counts (EWC)
EWC is a program that covers breast and cervical cancer screening services.
- We can assist you in applying for or renewing this coverage!
Coverages we do NOT accept:
Please see notes about EPO/POS/HMO commercial insurance under Private or Commercial Coverage above. We do not guarantee that we are in-network with any of these plans. If we are not listed as your primary care provider (PCP) on your insurance card, please call your plan to see if we are in-network or if you need a referral from your primary care provider to see us.
Kaiser
- We are not contracted with or in-network with any Kaiser plans. If you are new to Kaiser and looking for gender affirming care services, you can call Kaiser to get help access those services through them.
Family PACT (green HAP (Health Access Program) card)
- The Family PACT program provides coverage for some sexual and reproductive care needs, including pregnancy tests, STI testing, cervical cancer screening, and contraceptive options. The clinic is currently not contracted with Family PACT and is not able to help patients enroll in coverage.
- You can find a contracted provider here: https://familypact.org/provider-search/
- We are in the process of applying to become an FPACT provider, but this process is expected to take months before we are active and can assist you using this coverage.
Sin seguro
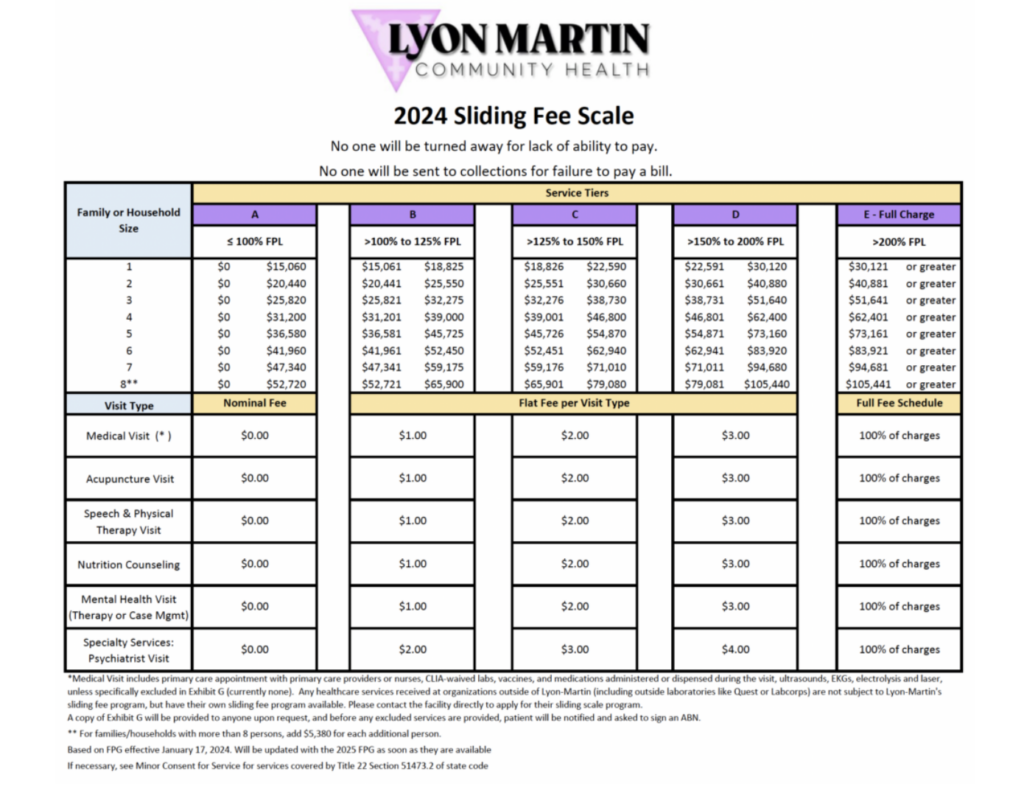
Lyon-Martin will never turn any client away for lack of ability to pay. We do not send anyone to collections for failing to pay bills. Clients without insurance will be asked to apply for our sliding scale, which allows for low-income clients to be billed at small flat rate fee based on income. If you do not have any income documentation, you may sign a letter self-attesting your income. Sliding scale applications should be completed within 30 days of your first office that will not be covered by insurance and are renewed annually.
We can enroll clients who are uninsured into coverage programs such as Healthy San Francisco (if you reside in San Francisco) and/or Every Woman Counts (EWC) to help pay for the cost of services at our clinic and for some referrals for specialty care.
As of April 1, 2024, our updated sliding fee scale is: